Quick tips: ABCs of cholesterol and other meaty topics
Hi from the mailbox!
Another great Healthy Matters show this week -thanks to the listeners who are up on a Sunday morning – getting dressed, eating breakfast, going to church, drinking their coffee – and tuning in to listen to me talk about fungus and pus. So a heartfelt THANK YOU to Healthy Matters listeners and for your terrific questions by text and phone.
If you have not heard the show yet, you can do so a few ways:
- Live radio broadcast: WCCO 8-3-0 AM dial – Sundays 7:30 a.m. Central
- Live streaming on your computer/mobile: WCCO.COM – Sunday 7:30 a.m. Central
- Podcasts for listening at your convenience – podcasts available here.
The whole shebang is sponsored by my organization, Hennepin County Medical Center (HCMC) in be-yoo-tee-ful downtown Minneapolis.
This week’s post features quick answers to questions I received on the show. These are quick and incomplete, so make sure to talk to your own doctor to learn more.
I’ll also be doing some video posts where I can answer questions by talking rather than typing . . . look for those soon.
From the Healthy Matters mailbag
Several questions this week about cholesterol numbers, like this one . . .
“My doctor recommended coming back in 6 months for repeat of cholesterol numbers and tweaking my lifestyle. Is there an alternative to statins?”
Short answer: Dyslipidemia, which basically means your cholesterol is out of whack, is a risk factor for developing cardiovascular problems in the future. Statins remain the medications with the most scientific evidence to prove that they work. There are alternatives, but none with such strong proof to back them up.
Longer answer:
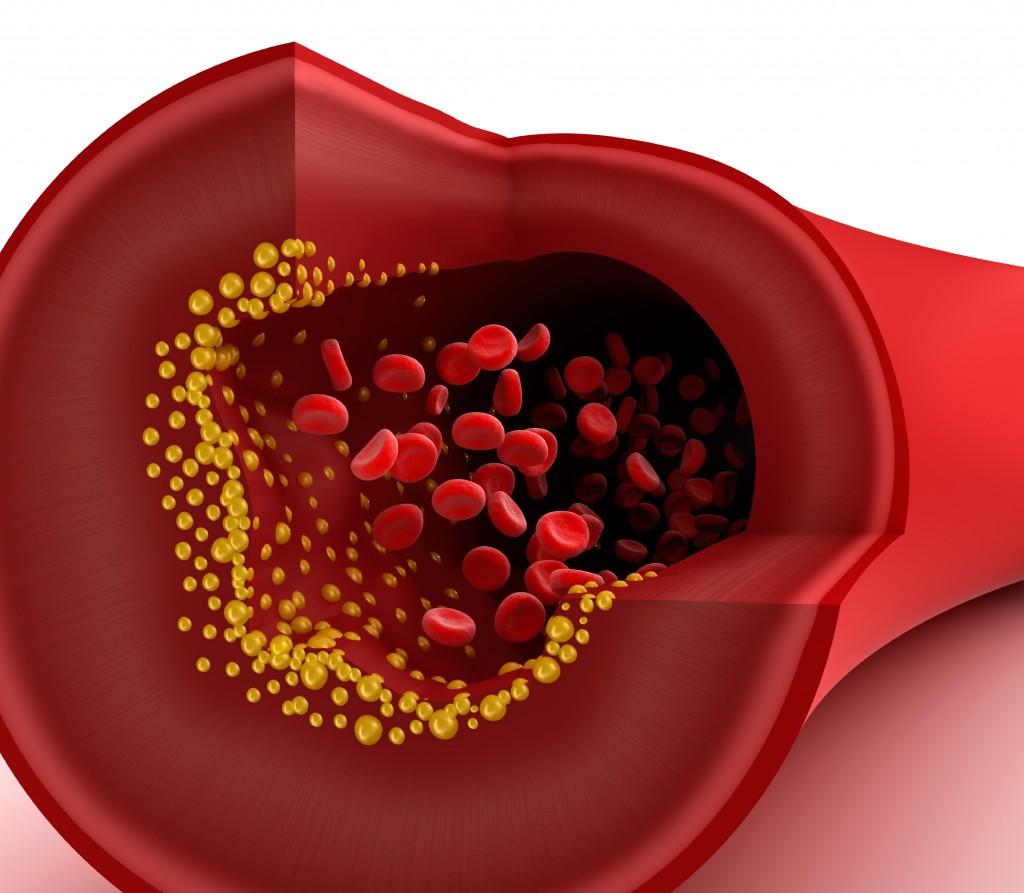
- LDL = low-density lipoprotein. LDL = bad. You want this one low.
- HDL = high-density lipoprotein. HDL = good. You want this one high.
- Triglycerides = fats floating around your blood stream. You want this low.
- Total cholesterol = a combination of the above (but you can’t simply add up the 3 of them to get your total cholesterol – it is a more complicated formula).
Your body actually requires cholesterol for life since it is part of cell membranes and an important part of the normal steroid hormones that your body makes. Most cholesterol is manufactured in your liver, with only a modest amount coming from your diet.
The trouble for many of us is that our cholesterol factories (aka your liver) don’t have an “off” switch. It simply makes too much. Think of statin medications as the “off” switch. Yes, they have side effects (the most common one is muscle problems) and as science progresses, we will undoubtedly learn more about these medications. But for now, for the right people, if you have cholesterol problems statins are the best way to reduce your risk of heart disease.
have an “off” switch. It simply makes too much. Think of statin medications as the “off” switch. Yes, they have side effects (the most common one is muscle problems) and as science progresses, we will undoubtedly learn more about these medications. But for now, for the right people, if you have cholesterol problems statins are the best way to reduce your risk of heart disease.
Who are the right people for statins? Here are the latest guidelines (new in 2015):
- People who do not have known cardiovascular disease and are between 40 and 75 years old and have a 7.5 percent or higher risk for heart attack or stroke within 10 years.
This is cool and you should do this –> to find out your 10-year risk of heart disease, click here.
- People with a history of heart attack, stroke, stable or unstable angina, peripheral artery disease, transient ischemic attack, or coronary or other arterial revascularization. (Basically if you have known cardiovascular disease).
- People 21 and older who have a very high level of bad cholesterol (190 or higher).
- People with Type 1 or Type 2 diabetes who are 40 to 75 years old.
There are a LOT of people who could be taking these medications and receiving the benefit of reduced risk of heart disease. Click here for a nice discussion of the guidelines.
Read on for another related question . . .
“I thought the higher the HDL cholesterol the better. My HDL was 100, LDL was 128, triglycerides 27. Doctor expressed concern that sometimes an HDL at either extreme can be a problem . . and ordered a VAP test.”
Here is an analogy that works for me. Bear with me, I made this up . . .

Think of LDL and triglycerides as “garbage” floating around your bloodstream and attaching itself to your blood vessel walls, like garbage accumulating on the curb.
Too much garbage = a mess of badness.
Now think of HDL as the “garbage trucks” driving around, picking up the garbage from the curb (vessel walls), and delivering it back to your liver where it can be processed and removed.
You want lots of garbage trucks.
So in general, you want an HDL that is high (preferably 50-60 or more). But can it be too high, as this questions asks? Well, yes, it is true that HDL that is not working properly is not only ineffective in its garbage truck duties, but may actually be harmful. However, we really don’t know what to do with that information.
The VAP test is a series of advanced tests that can more accurately pinpoint your cholesterol situation. As I mentioned on the radio, however, we still don’t know what to do with the information since getting the test will usually not lead to any change in treatments. After all, we don’t really have any additional proven treatments. So you can get the VAP test if your doctor recommends it, but be prepared to hear the same advice when it is back: eat healthy, exercise, don’t smoke, take a statin if indicated.
And choose your parents carefully.
On to a new topic from the mailbox . . .
“Do acid control medications cause Alzheimer’s Disease?”
Short answer. We don’t know.
Longer answer: This one has been in the news as of late since a group of German researchers published the results of their study which showed an association between proton-pump inhibitor use (PPI) and the development of dementia. The study was in people over 75 who did not have dementia at the outset, but who were taking one of the common acid-suppressing agents called PPIs. Examples (among many others) of these drugs are omeprazole (Prilosec) and lansoprazole (Prevacid).
The study showed that more people on these medications developed dementia than those not taking them. Why this may be the case is not known. But it is really important to note that the association between these medications and dementia is not proof of causation. In other words, these medical studies do not prove that doing one thing (taking the acid-suppressing medications) actually causes the other thing (getting dementia). Here’s a link to the actual study if you are super into medical journal articles with subtitles like “A Pharmacoepidemiological Claims Data Analysis” – I’m not joking, that is the actual subtitle of this real page-turner.
Bottom line: this is not a reason to stop taking your acid-suppressing medications if you have a strong indication to do so (you have proven acid-reflux disease, for instance). I should add that many people take acid-suppressing medications for shakier reasons and probably don’t need them in the first place.
One more for the good measure . . .
“Paryonychia on thumb. Causes?”
Paronychia is an inflammation around the finger- or toenails. It is sometimes chronic (long-lasting) but often acute (comes on quickly and resolves). It is usually due to a bacteria or fungus getting in the grooves around your nails. It shows up as a sore, red, and swollen area around the nail. The acute kind may be due to minor daily-living types of activities (dishwashing, trimming nails, minor trauma . . . ) and may not need any specific treatment other that putting warmth or topical anti-inflammatories on it.
If there is pus oozing out of it, you may need antibiotics or drainage by your doctor. Chronic paronychia may be due to a fungal or allergic type of dermatitis, and may require topical treatments with anti-inflammatories or anti-fungals.
The rest of the mailbox
To give you a sense of the range of topics on a typical Healthy Matters Open Lines show – I’ll show you a partial and condensed list of the topics listeners raised this week but that I did not get to cover. I’m struck by the range of questions – and also just how legitimate they all are! Doing the radio show really makes me aware of the shared human condition – I bet most of us can relate to something on this list . . . !
- Febrile seizures in infants.
- What is neuropathy?
- Clostridium difficile infections.
- Atrial fibrillation.
- Cold sores in a young adult.
- Epilepsy in children.
- Ear infections.
- Testing for Diabetes type 2.
- What is pre-diabetes?
- Causes of dry tongue?
- Carpal tunnel syndrome.
- High calcium in blood tests.
Keep listening, keep checking out the blog . . . and if you have a preference for what I should cover in the future please leave me a comment and I’ll do my best!
Diabetes care and research with Dr. Elizabeth Seaquist
If you missed the show this morning about diabetes with Dr. Elizabeth Seaquist from the University of Minnesota, you’re going to want to check out the podcast. She is not only a terrific person to hang out with but she is also incredibly accomp lished in her career as a clinician and researcher. And she is terrific at explaining diabetes, why it matters, and how she and others are doing research that promises to help us all in managing diabetes into the future. No, that is not Dr. Seaquist in this picture (I think it is Hesy-ra, the Egyptian who first described diabetes in 1552 BC). I was going to take a selfie of Dr. Seaquist at the microphone but alas and alack, I forgot. Here’s her bio page at the University of Minnesota. There is a short video from Dr. Seaquist later in the post as well.
lished in her career as a clinician and researcher. And she is terrific at explaining diabetes, why it matters, and how she and others are doing research that promises to help us all in managing diabetes into the future. No, that is not Dr. Seaquist in this picture (I think it is Hesy-ra, the Egyptian who first described diabetes in 1552 BC). I was going to take a selfie of Dr. Seaquist at the microphone but alas and alack, I forgot. Here’s her bio page at the University of Minnesota. There is a short video from Dr. Seaquist later in the post as well.
For those of you checking for information about the GRADE study that we discussed on the air today, the number is 612-301-7040 or grade@umn.edu for the University of Minnesota location. Read more about GRADE later in this post.
And I’ll do a couple quick tips from the phone and text line at the end of this post. OK, on to the business of honey sweet urine. Ew.
Sweet urine
First I can’t resist a quick aside about the origins of the name “diabetes mellitus” (which is the full name of the disease). Diabetes is from the Greek for “siphon” (or “passing through”) and mellitus from the Latin for “honey” or “sweet.” Put ’em together and it loosely means “sweet urine” – sugar passing through the body and kidneys into the urine. Ancient people were aware of what was probably diabetes in Egypt, China, India, Persia, and Greece, but it was an intrepid British doctor who really latched onto the sweetness of urine (and now for the “ew” factor – I guess that they used to actually taste the urine. Makes one immensely thankful for modern lab equipment).
OK, enough history.
Diabetes basics
For Type 1 diabetes, the body lacks the normal function of creating insulin, which is necessary for life. This is the less common form of diabetes and it always requires insulin for treatment. I’m not going to talk about it here.
Type 2 diabetes is in some ways more complex and thus harder to summarize. Basically, the body creates some insulin, but it is either in insufficient amounts or the body is resistant to the usual effects of insulin. This is called insulin resistance. It correlates with excess body weight, so being overweight does put one at higher risk for developing diabetes (and conversely, diabetics who can lose weight can improve their sugar control). However, as Dr. Seaquist mentioned on the show today, there is more to the story than being overweight, something that should be evident when you consider that some lean people develop diabetes while many overweight people do not. So there is a genetic component that we are still trying to understand.
Diabetes is such an important topic that people spend their whole careers diagnosing, treating, researching, and support patients with diabetes. It is certainly too much for a blog post. I would refer you to the American Diabetes Association for solid information. Just a couple of points here.
If you have Type 2 diabetes, you should:
- Know your A1c and your A1c goal (usually aim for <7%, but this can vary with your personal situation so ask your doctor).
- See your doctor regularly (every 3 months, or more frequently if sugar control is not adequate).
- Manage your glycemic control (aka sugars) with diet and exercise, and if that is not enough to reach your A1c goal, then with medication.
- Pay attention to the parts of yourself that are vulnerable – get eye exams, protect your feet and wear good shoes, monitor your kidney function, and do what you can to lower your risk of heart disease (keep cholesterol down, consider taking an aspirin a day, do not smoke . . ). Of course, these are general guidelines only – you should do all of this in consultation with your doctor.
- And finally, consider enrolling in the GRADE study if you meet the criteria
GRADE study
There are oodles of treatments that are FDA-approved to manage Type 2 diabetes. A healthy diet and exercise are important for everybody After that, the first choice for most people will be a medication called metformin. Medical data has shown that this is the most effective at safely bringing blood sugars under some control.
The problem is that for many people, metformin alone does not control the high blood sugars adequately. In other words, metformin alone does not bring their glycosylated hemoglobin, or A1c below ~7%. (You may have a slightly different goal based on factors unique to you, but for most people getting below 7% is a good goal). So a second agent is needed, and that’s where there is not rock-solid data to tell doctors and patients what to use next. Is it insulin? One of the older classes of drugs called sulfonylureas? Or perhaps one should use some of the newer drugs, of which there are many. After all, they are all FDA-approved, but after metformin we still don’t know which ones are best.
So that is the big question that the GRADE study is going to help us answer. Check out the short video about GRADE:
https://youtube.com/watch?v=2KGjmtevQKk%3Frel%3D0%2520frameborder%3D0%2520allowfullscreen
If you have diabetes type 2, ask yourself these 2 questions:
- Have I had diabetes less than 10 years?
- Is metformin my only diabetes medication?
If the answer is YES to both of these, then you may qualify for the GRADE study. If you enroll, you can expect the following:
- Ongoing care at the University of Minnesota (in Minneapolis, or at another GRADE site near you) for medical visits 4 times per year.
- You will get your diabetes medications at no cost to you.
- You will get your physical exam and diabetes lab tests also at no cost to you.
Great care for your diabetes, free tests and medications, and you will be doing an important service to people living with diabetes everywhere by helping us all understand the best treatments. I encourage you to give the GRADE researchers a call. Their University of Minnesota number is 612-301-7040 or e-mail them at grade@umn.edu. If you live elsewhere, go to the GRADE site at gradestudy.com to find a location in your part of the country.
I really want to thank Dr. Betsy Seaquist for joining me this morning. HCMC and the University of Minnesota are partners in clinical care and research!
Quick tips from Healthy Matters text line
I received way more questions from listeners than I can answer on the air Sunday mornings. Here are short responses to a few text questions from today (I paraphrase the questions a bit here).
Is macular degeneration the eye condition associated with diabetes? Although macular degeneration is a common eye condition, it is not the one we most associate with diabetes. Diabetes does lead to a higher risk of retinopathy (sometimes with excess blood vessel growth in the eye), macular edema (swelling in the back of the eye), cataract, and glaucoma. These are treatable conditions, so people with diabetes should get regular eye exams.
Is it possible to stop taking diabetes medications if I lose weight? For many people, yes, this is not a myth. Sometimes losing just 10-20 pounds may be enough to control blood sugars. Certainly there is strong evidence that people who are very overweight and then get a weight-reduction surgery often are able to stop their diabetes medications almost right away.
Can prednisone raise blood sugars? You bet it can! We touched on this on the radio today a bit. Any corticosteroid (like prednisone pills that you swallow, or intravenous steroids that some people in the hospital need, or even injections into your knee or other joints) can and usually do raise your blood sugar levels. Usually the blood sugar levels come down after these anti-inflammatories are stopped, but be prepared to adjust your diabetes medications if you are also on these corticosteroids. As always, consult your doctor before changing any of your diabetes medications and be sure to let your doctor know if you need to take these steroid medications.
Healthy Matters – next week on the radio: Open Lines! Get your general health questions ready.
Reflections on bias in health care
Do black people feel less pain than white people? Are overweight people at fault for developing diabetes? Do doctors evaluate symptoms differently if a white man reports them than if a black woman reports them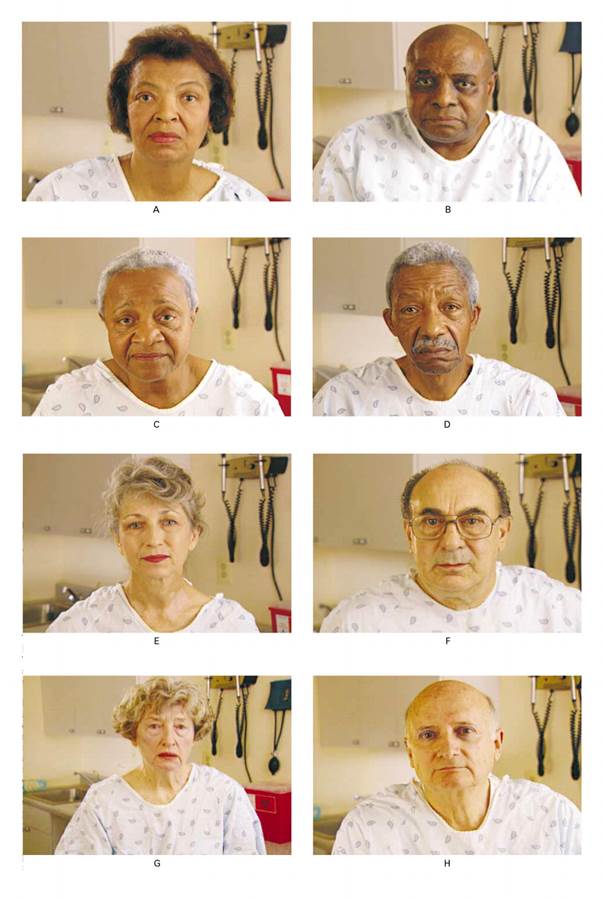 ?
?
Most of us would emphatically answer these no, no, and no. But there is evidence that the answers actually are much more complex than that. For instance, there is scientific data that suggests that people hold unacknowledged attitudes that African-Americans feel pain less than white people. Some people do feel that overweight people are personally to blame for their diabetes. And there are studies that suggest that doctors evaluate and treat people differently based on race. (The punch line of the study is that when the actors in this picture reported symptoms to doctors, they received different treatment recommendations despite identical symptoms – a fascinating study).
I think these are disturbing but important things to think about if we are going to address disparities in health care.
This post is prompted by a class that I facilitated at the University of Minnesota Medical School. I was pinch-hitting for a colleague this week in a small-group discussion class that that aims to get these first-year medical students to think about something other than biochemistry and physiology. Stuff like bioethics, humanistic care, doctor-patient relationship, and so forth. There were ten of us seated around a table discussing the week’s topic – bias in medical care. (As an aside – if these 10 thoughtful students are any indication – the future of health care is in good hands.)
I’d like to share some reflections from that session and offer some interactive resources for you to try – the exact same ones the students did. And you don’t have to pay medical school tuition! So read on, think about it, check out some of the links, examine your own biases, and leave a comment on this blog post. Let’s talk about it.
(At the bottom there is a link to a thought-provoking self-assessment that you may wish to consider doing yourself).
Being privileged
I think the first step toward addressing bias is to examine our own situation. Here is my situation, in the proverbial nutshell:
- White
- Male
- Straight
- Financially secure
- Naturally-born United States citizen
- Protestant Christian
- English-speaker
- Not overweight
I don’t apologize for any of them – I am happy with who I am. But it is crucial to realize that I didn’t do anything to accomplish any of those things – and yet, my personal characteristics put me in a place of privilege. Nobody would doubt me if I showed up in an Emergency Department with chest pain. I’d get the appropriate tests in an instant and probably be provided with pain medications without delay.
Would I get the same great medical care if I were a disheveled homeless man? If I didn’t speak English? If I were a Muslim woman wearing a hijab? If I were a transgender person? If I were a woman? If I were overweight? Maybe, maybe not.
So we talked about this with the medical students, starting with recognizing one’s own privilege and naming it out loud. I told the students, especially the white guys, that it is totally OK and cool to be a white guy. No apologies. But it is important to recognize the privilege that comes with personal characteristics which you were simply born into.
Great quote: “When you find yourself on 3rd base, don’t assume you hit a triple to get there.”
Unconscious bias vs. conscious bias
What is bias, anyway? The medical students in our class watched the following video of a talk given by a physician who reflects on his own bias. It is worth 15 minutes of your time:
[ted id=1774]
This video raises several points to ponder, but two stick out for me. First, Dr. Attia painfully recalls the contempt for which he held a diabetic patient – basically blaming her for needing a leg amputation because she was – as he recalls – “fat” and therefore somehow responsible for her decaying leg. Years later he still feels the need for her forgiveness for this attitude that he wasn’t even aware of at the time (be sure to watch it to the end). The second point is his recognition that medical science may, in fact, not always be accurate. This second point is certainly true and something I hope to explore in future posts. The first point is a perfect example of bias.
In our medical school discussion, we tried to acknowledge the possibility that we could be harboring bias even without knowing it – implicit or unconscious bias as opposed to explicit or conscious bias.
Explicit bias
First the one that is easy to identify – explicit bias. This is something we deliberately think about and often verbalize. Consider the current United States presidential campaign, when serious candidates for the presidency are endlessly providing examples of explicit bias: accusing whole groups of people of nefarious deeds (Mexican people as rapists), labeling hundreds of millions of people into stereotypical categories (lumping all Muslims together), openly advocating mass killing of innocent people for being not like us (“carpet-bombing” whole populations of civilians).
These are open, deliberate attitudes that should be easy to identify and weed out (although sadly we often fail at this). I would call them explicit biases and we should reject them outright.
Now the harder one. Contrast explicit bias to implicit (or unconscious) bias. These are the attitudes that we are not conscious of and that we may well deny holding when confronted with them. But they are real. Like Peter Attia in the Ted talk (click picture above if you missed it), I would never openly accuse a person with diabetes of being personally responsible for her gangrenous leg. But deep inside me, would a part of me wonder if she could have tried harder to lose weight? If she had only cared for her leg a little better could she have avoided an amputation? I think that it is not only possible that I could hold such unconscious biases, I think it likely that I do. And most of my physician colleagues do as well.
This part is hard . . . examining our own bias
The medical students were asked to take a self-assessment, called an IAT (Implicit Association Test). My first reaction is that the IAT is just another bit of academic jargon, but having tried it I found it actually sort of cool. The test involves words and images appearing on the screen, and the students are asked to rapidly react to the images by making a selection. No thinking about it logically. Just react.
I encourage you to try an IAT – take a test yourself. This can be difficult emotionally, so prepare yourself. Hearing your own results may not be easy but it is eye-opening. Before you take a test, read the materials from the Implicit project (a consortium of researchers) on the website and then take the test yourself. Note that the interpretation of your results may be troubling to you. With that in mind – give it a try.
Did you discover any unconscious bias in yourself? How did it make you feel to hear that you may harbor attitudes that you were not aware of? Do you agree that such biases exist in you? And if so, what ought we to do with that information? How is our society affected, not only in healthcare, but in other aspects of our life, when such biases exist? Does bias contribute to unequal health care outcomes?
This is a conversation worth having. Tell me what you think – leave me a comment!


