The stethoscope of the 21st century?

Credit: Wellcome Library, London. Wellcome Images
http://wellcomeimages.org
René Théophile Hyacinthe Laënnec auscultating a tuberculous patient at the Necker Hospital, Paris. Gouache after T. Chartran.
“That it will ever come into general use, notwithstanding its value, is extremely doubtful; because its beneficial application requires much time and gives a good bit of trouble both to the patient and the practitioner; because its hue and character are foreign and opposed to all our habits and associations.”
Such was the opinion of the stethoscope by an English doctor in 1821 named John Forbes. The stethoscope had recently been invented by French physician René-Théophile-Hyacinthe Laënnec in an effort to protect the modesty of his female patients by removing the necessity of placing his ears directly against their chests. The skepticism of Dr. Forbes notwithstanding, the stethoscope is now considered one of the greatest inventions in history. Check out the patient of Dr. Laënnec at the left – head firmly pasted to the chest of this guy with tuberculosis. Oh my! (Since this patient was male, the good doctor did not need to use his new stethoscope invention).
Whether the doctor actually contracted tuberculosis I know not.
But in the year 2016, the stethoscope is so familiar to patients that we probably would wonder what was wrong if the doctor did not have one hanging around his or her shoulders. 
So what is the technology that doctors will be using in the future?
Enter the ultrasound
The stethoscope is nearly 200 years old. Although I doubt I’ll ever hang my stethoscope up for good, today we do have some newer tools to help with diagnosis. The ultrasound, though a tool we have had for many years, has now hit the bedside. Today I spent some time with my colleagues (inpatient doctors, or hospitalists) learning how to use portable ultrasound machines in our practice. As a patient, you will likely encounter a doctor with an ultrasound in his or her pocket and you may wonder what the heck this is all about.
So this post is a sort of “mini-Medical School” into the use of ultrasound in clinical diagnosis – a brief look at how clinicians of today can use this tool in medical practice.
Most medical students are repeatedly taught that 80% of the diagnoses they make on their patients will be from the history and physical exam. In other words, fancy blood tests, high-tech imaging (x-rays, CT, MRI . . . ) and other extensive tests are needed much less often than we all may think – perhaps just 20% of the time. So we teach doctors-in-training to learn the skills of talking to patients and laying on of hands by doing a physical exam. Most of us can recall some of our mentors and teachers, patiently and skillfully showing us the tried-and-true physical exam skills.
An anecdote from my training about one of the great ones . . . I remem ber Dr. Richard Asinger, here at HCMC, putting his stethoscope on the top of a patient’s head. I thought he was messing with me, but he said he could actually hear a heart murmur up there. I was in awe of this pure genius. On the other hand, maybe he really was just messing with me! He’s still at HCMC; I should go ask him. On a side note, he’s also a killer dancer on the dance floor.
ber Dr. Richard Asinger, here at HCMC, putting his stethoscope on the top of a patient’s head. I thought he was messing with me, but he said he could actually hear a heart murmur up there. I was in awe of this pure genius. On the other hand, maybe he really was just messing with me! He’s still at HCMC; I should go ask him. On a side note, he’s also a killer dancer on the dance floor.
But even listening with our stethoscopes to hear abnormalities of the heart (murmurs, for instance, which could mean valve disease) , or of the lungs (like rales, which could mean pneumonia) it is still a bit primitive. Sometimes we want to know how much extra fluid a person has in their body due to heart failure (called hypervolemia). Or we need to know if they have a partially collapsed lung with air around it (called a pneumothorax). Or if they have a blood clot in their legs (called a deep venous thrombosis, or DVT).
So that is where ultrasound comes in.
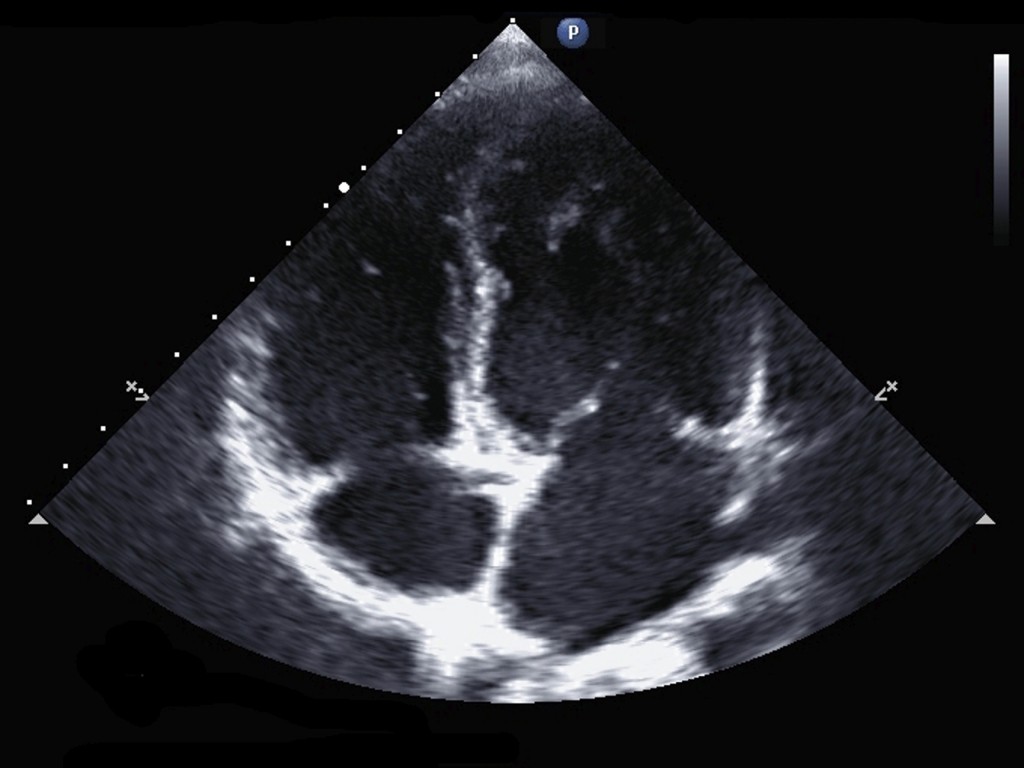
This is an ultrasound image of a heart.
- See the four chambers? Clockwise from upper left: right ventricle, left ventricle, left atrium, right atrium.
- See the valves? There are four valves in your heart – you can really see the mitral valve leaflets in this picture – the two white lines that look like a tent at about the 3:00 position.
If the chambers and vessels look big – maybe you have too much fluid in your body. If the valves are not opening and closing correctly, maybe that is what is causing that murmur we hear with our stethoscope. If the heart is not beating strongly, you may have heart failure. So much information can be learned from these pictures!
Ultrasound training with the HCMC Hospitalists
I thought Healthy Matters listeners and blog readers may like to see how we stay competent in the medical profession – so here’s a sneak peek of our group at HCMC learning to use ultrasound in our daily practice. The technology is really neat. The machine is just a bit bigger than your smartphone, so now we can carry them around in our white coat pockets. I think you will see more and more of this when you are a patient – doctors pulling out teeny little ultrasound machines. I have even heard that we will be able to use our smartphones for this purpose at some point.
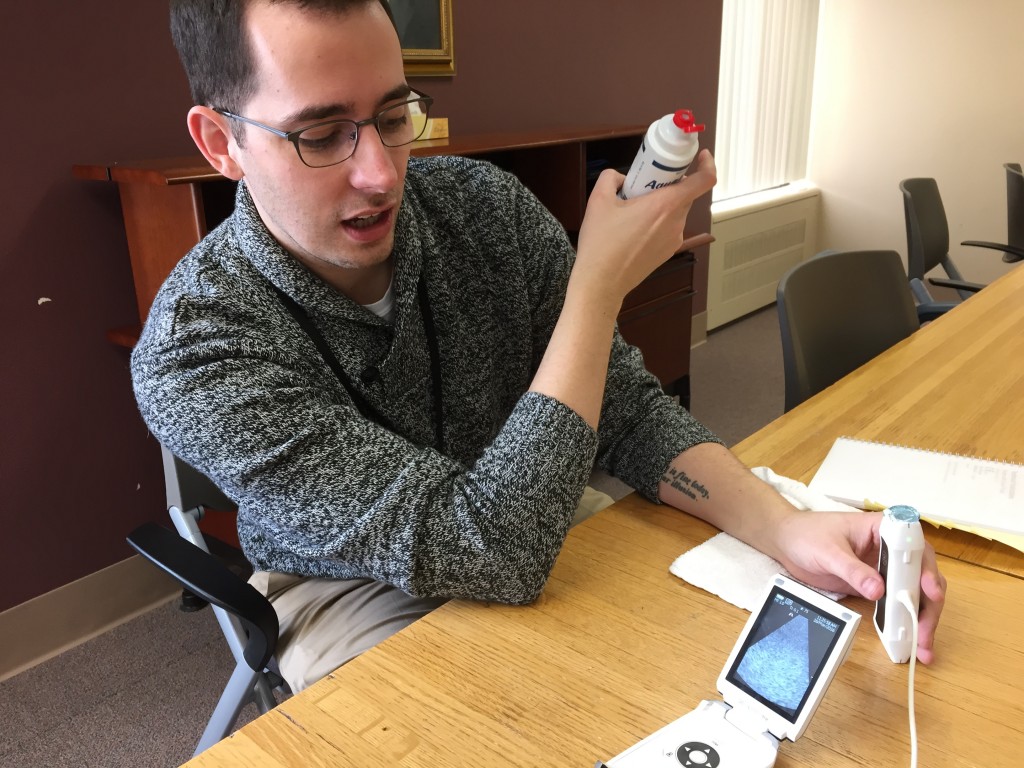
Here’s my colleague, Dr. Mike Lawson – an HCMC graduate, all-around good guy, and Minnesota Vikings fan – recently returned to Minneapolis after a spell as a doctor in the Seattle VA Medical Center. He’s really good at using ultrasound and one of the best teachers around so he was helping the rest of us become proficient at it.
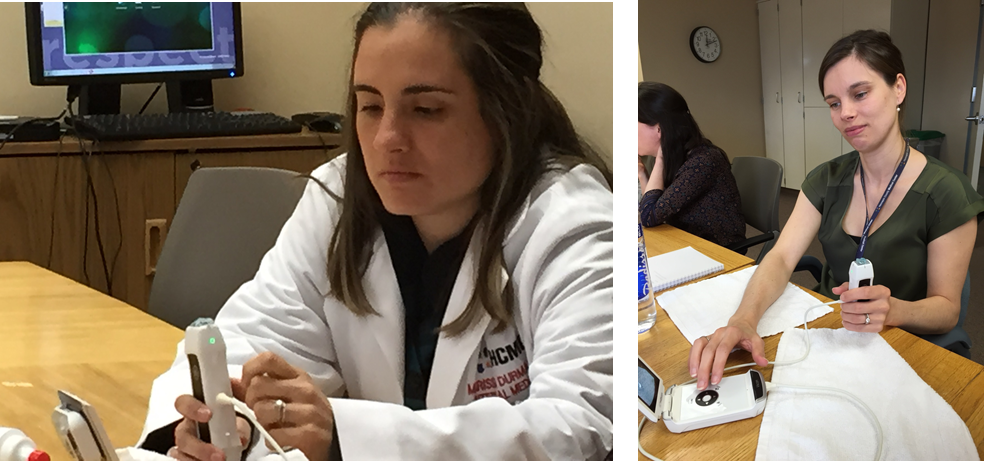
These pictures are of two of our outstanding clinicians working with the ultrasound machines (Chief Resident Dr. Marissa Durman on the left and Physician Assistant Erica Monroe at right). Look at how tiny the machines are! The doctors and PAs in our group were worried that they were going to have to do ultrasounds on pregnant women. No worries – we have specialists for that! Relief all around.
From putting an ear to a patient’s chest to listening through the tubes of a stethoscope to using sound waves on a portable ultrasound.
The centuries-long attempt to probe the human body continues.
When weight loss surgery makes sense
“O
nly 1-2% of people who could benefit from weight loss surgery are actually getting it done”
So says Dr. Gil Hartley, my radio guest this week on Healthy Matters. Dr. Hartley is an internal medicine physician, like me, who specializes in the care of people who are very overweight. We focused our conversation on bariatric surgery – which is the medical term for weight loss surgery.
Here is the Healthy Matters podcast page to listen to this show or any of our recent shows.
 The first step to knowing if weight loss surgery may be right for you is to calculate your own Body Mass Index, or BMI. You just have to know your height and weight, and it takes less than a minute to do. Find out your BMI by clicking the button —>
The first step to knowing if weight loss surgery may be right for you is to calculate your own Body Mass Index, or BMI. You just have to know your height and weight, and it takes less than a minute to do. Find out your BMI by clicking the button —>
What does the BMI mean
Here are the categories of BMI:
- <18.5 = Underweight
- 18.5 – 25 = Healthy weight
- 25 – 30 = Overweight
- 30 – 40 = Obese
- >40 = Severely obese
It may be emotionally hard to find out which category you fall into – and you’d be right to note that it is just a number. But think of it as a starting place, and if your BMI is high, perhaps now is the time to take action. Especially if your BMI is greater than 40 in which case I really encourage you to see a weight loss surgery expert. For people with diabetes, the BMI at which to consider surgery drops to 35.
Is weight loss surgery right for me?
As Dr. Hartley mentioned, weight loss surgery is the best option for many people who are excessively overweight – the people who are at risk for complications due to their weight – diabetes being the most prominent example but also including high blood pressure and obstructive sleep apnea. I won’t get into all the details, as there are lots of good resources for people who are overweight or obese (for instance, check here for good info from the National Institutes of Health – a source you can trust). But what struck me about my conversation with Dr. Hartley was when he said the resistance of people to getting weight loss surgery is still a real problem. And he isn’t trying to peddle unnecessary surgeries on anyone. He simply knows firsthand that surgery is the best solution for many people.
And don’t be too hard on yourself. Being overweight is not a character flaw. For most people, it is also not just a problem with overeating (although that is the problem for some). Rather, obesity is a complex chronic condition with lots of causes and contributing factors.
I’ll close with a few more things I learned from Dr. Hartley today about weight loss surgery:
- Weight loss surgery may be the most effective treatment for diabetic patients who are obese. Some patients actually leave the hospital after the surgery without needing their diabetes medications anymore!
- We used to think it did not matter when you did your surgery. We told people to just think about it and do it whenever you are ready. Doctors are reconsidering this due to more recent evidence that suggests that getting it done earlier leads to better longer-term health in patients with diabetes. So waiting for years and years to do the surgery may not be the best idea after all.
- The laparoscopic banding surgery, which showed great promise 10 years ago, is used much less today. The two more common surgeries are gastric bypass (Roux-en-Y), and vertical sleeve gastrectomy.
- You can drink liquids without problem after weight loss surgery. One caller to the show was worried about being thirsty after surgery. Not to worry, you can still drink liquids normally as they just pass through your system just like they always did before surgery.
- Loose skin can be a problem for some after weight loss surgery (to the degree that cosmetic surgery is considered), but for many people the skin does remodel back to a less bothersome condition over time.
If you are in Minnesota and want to take action on your weight . . . here is information on Dr. Hartley and his team at the Hennepin Bariatric Center.
Thanks for joining me on the air, streaming online, and on MyHealthyMatters.org!
Every 8 seconds: the science of brain injury with Dr. Uzma Samadani
There’s big news from HCMC this week. Many know that HCMC is the largest provider of TBI care in the state of Minnesota. But many don’t know that we are also a major research institution and in no area is this more true than TBI.
The big news is that our researchers are launching the largest single-center study of brain injury in the United States. It’s been all over the news – check out the buzz this is getting in the national media.
Eye tracking
Every 8 seconds someone has a traumatic brain injury. But you may be surprised to learn that doctors really don’t have great answers to the most basic questions like:
Do I have a brain injury? How bad is it? Where is it in my brain?
That is what the researchers hope to answer.
Shakira’s hips
Shakira’s hips? Huh? Rather than have me try to explain it – watch this brief talk by Dr. Samadani herself. It is fascinating.
So Dr. Samadani and her team are doing research based on the knowledge that you can actually track the movements of a patient’s eyes to help answer these questions. As it is now, doctors wave their finger in front of a patient like we have been doing for centuries. The researchers are hoping to change that by studying all sorts of ways to diagnose brain injury – using blood tests, eye tracking, and imaging (x-rays and pictures and the like) . The eye tracking technology in particular could be game-changing in the way we diagnose and treat brain injury. For more on eye tracking, click here.
I am convinced that some day the research being done right here at Hennepin County Medical Center and the University of Minnesota will change the lives of millions of people.
That excites me!