Hi, everybody and thanks for stopping by. This is Part 2 of our look at diabetes, aided by my colleague, endocrinologist Dr. Laura LaFave. Click on Part 1 here if you missed it from last week.
In this part, I’ll cover:
- Risk factors for developing diabetes. (Includes a BMI calculator that you should try).
- Complications of diabetes.
- Tips for reducing your chance of getting diabetes.
Here we go!
Risk factors: what leads to diabetes?
We know that Type 1 diabetes is caused by the failure of certain cells in the pancreas to make insulin. Insulin is necessary for life and so if the body doesn’t make any, that causes diabetes.
But that’s type 1, which is <5% of the cases of diabetes. The other 95% is type 2 diabetes, and there is no single cause for type 2. In fact, we’re not really sure what causes it at all. What we do know is that there are risk factors which raise the chances that a person will develop type 2 diabetes. A risk factor is not a direct cause necessarily. Example: being overweight is a risk factor for developing diabetes, but at the same time, not all overweight people have diabetes.
Dr. LaFave, when she was on Healthy Matters a couple weeks ago, talked to us about risk factors. You can listen to her yourself on the podcast here. Here’s a brief summary of what she said:
Diabetes risk factors
Age over 45 years. Older folks develop diabetes at higher rates, and so we use the somewhat arbitrary age of 45 as a starting point. At age 65, fully 25% of people have diabetes.
Obesity or being overweight. This is well-established risk for diabetes and is the one we talk the most about. It is simply a fact that if you are overweight, your chances of getting diabetes is higher. One way to measure this is the Body Mass Index, or BMI. A BMI over 25 is called overweight and puts you at higher risk for diabetes. For people of Asian descent, the BMI cutoff is lower, so if it is greater than 23 in person of Asian origin, that is a risk factor.
If you don’t know your BMI, I encourage you to check it by clicking on this BMI calculator. You just need to know your height and weight.
Family history. If you have first degree family members with diabetes (parents, siblings, children) then you are at higher risk for developing it yourself.
Gestational diabetes. Women who had gestational diabetes (diabetes of pregnancy) have a 50% chance of developing diabetes 10 years after that pregnancy. Even if the diabetes went away after the pregnancy (as it usually does) women in this group should be tested for diabetes frequently (like every year).
Ethnicity. Certain populations face higher rates of diabetes than others. The reasons for this are complicated and may have to do with lots of factors that we don’t understand (like poor access to health care, nutritional, environment, poverty, maybe genetics, and such things). Here is a sampling of diabetes rates in the United States:
[table id=9 /]
Complications of diabetes. What goes wrong.
With a couple exceptions, the dangers of diabetes are not immediate. Those exceptions are 1) hypoglycemic which is low blood sugars, and 2) ketoacidosis which is a severe condition of very high blood sugars. Both problems are emergencies. But most problems with diabetes happen 5 or 10 years – or even later – down the road.
Complications can be lumped into two big groups: microvascular and macrovascular.
When glucose accumulates in the blood stream, it is useless to the cells where it is needed, and instead, it wreaks havoc with the blood vessels. The sheer number of complications from this simple problem – too much circulating glucose – may surprise you. Here’s a sampling of what can happen.
The small blood vessels, microvascular complications
Microvascular complications affect body organs that have itty-bitty blood vessels supplying them. Here are the big three.
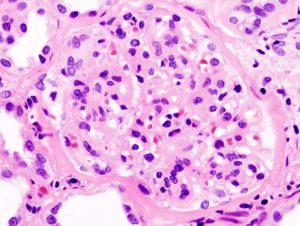
In the kidneys the condition is called nephropathy. Each kidney is made up of literally millions of tiny tubules called nephrons (hence the field of kidney disease is called nephrology). Nephrons, although microscopically small, are complex tangles of blood vessels, cells, and tubes to carry urine. Diabetes destroys that delicate structure, leading to poor filtering by the kidneys, and eventually kidney failure. This requires dialysis, or more effectively, kidney transplant.
Similarly named but entirely different is neuropathy. The nerves which go the longest are the ones to a person’s feet and to a lesser degree the hands. When diabetes is long-standing, these nerves get damaged. The result is decreased sensation to the feet which is called neuropathy. If the person isn’t vigilant it can lead to wounds that the person can’t even feel. A bad spiral can then occur where the wounds get infected and may lead to amputations.
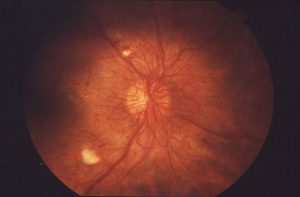
The third complication is retinopathy. This is the leading cause of blindness in the US and it is a result of damage to those tiny blood vessels in the back of the eye. It turns out that too much sugar leads to an overabundance of those blood vessels which leads to blurry vision and sometime blindness.
All three of these complications can be delayed or even prevented with good blood sugar control!
What about the big blood vessels?
Too much glucose is also bad for the large blood vessels, mainly the ones supplying the heart and brain. The reasons are not entirely obvious, but it is well-established that the risk of getting coronary artery or cerebrovascular disease (which cause heart attack and stroke) are much higher in people with diabetes.
Tips for preventing diabetes
So what can a person do to lower the risk of developing diabetes?
The biggest steps you can take are in weight control.
The top step a person can take is to get to a healthy weight. This is admittedly easier to talk about than to pull off in real life. But it is a fact – every extra 5-10 pounds you are carrying increases your risk of developing diabetes at some point. The medical studies are pretty clear on this point. One such study shows that for those with pre-diabetes, the risk of progression to full-blown diabetes goes way down with a loss of 5-7% of body weight.
The advice may sound familiar but bears repeating:
- Eat a balanced diet of vegetables, fruits, meats if you wish, whole grains, and legumes.
- Avoid refined sugars as much as you possibly can. There is nothing healthy about sugar in food sources such as soda pop, energy drinks, candy, and such.
- Limit simple carbohydrates (the four big culprits are the “white” foods: potatoes, pasta, rice, and bread). Stick to complex carbs like vegetables and whole grains.
- Limit saturated fats, like solid vegetable shortening. Other fats aren’t probably so bad – like olive oil, fish oils, even butter in reasonable portions.
- Limit portion size. We eat simply way too many calories for the most part.
- Exercise! You don’t have to go to an expensive gym every day. Walking, running, gardening, shoveling, dancing . . . whatever! Shoot for 150 minutes per week of moving, with 75 minutes of higher intensity activity per week. That isn’t all much if you try.
- Take the stairs, not the elevator.
For lots more information about diabetes, check out the reliable American Diabetes Association.
I hope you found something useful in these Diabetes posts. My big thanks to my colleague, Dr. Laura LaFave, for helping us out. By the way, Dr. LaFave is seeing patients at our spiffy Clinic and Specialty Center. Click on Hennepin Healthcare to make an appointment.
David