A doctor’s diary from a pandemic: Caring for the caregivers
 Many of you have reached out to me and my colleagues in healthcare with words of support, thanks, and encouragement. It means more than you know that the doctors and nurses and therapists and mental health workers and cafeteria workers and housekeeping staff – all of us – get uplifted in the hearts of our community.
Many of you have reached out to me and my colleagues in healthcare with words of support, thanks, and encouragement. It means more than you know that the doctors and nurses and therapists and mental health workers and cafeteria workers and housekeeping staff – all of us – get uplifted in the hearts of our community.
Speaking for the physicians (and the nurses, I’m sure) . . . we all went into this to be of service to others, and indeed, we all did “sign up for this.” But nobody expected to work with this level of anxiety. Nobody expected the level of worry that we may be exposing our families. Really nobody expected any of this.
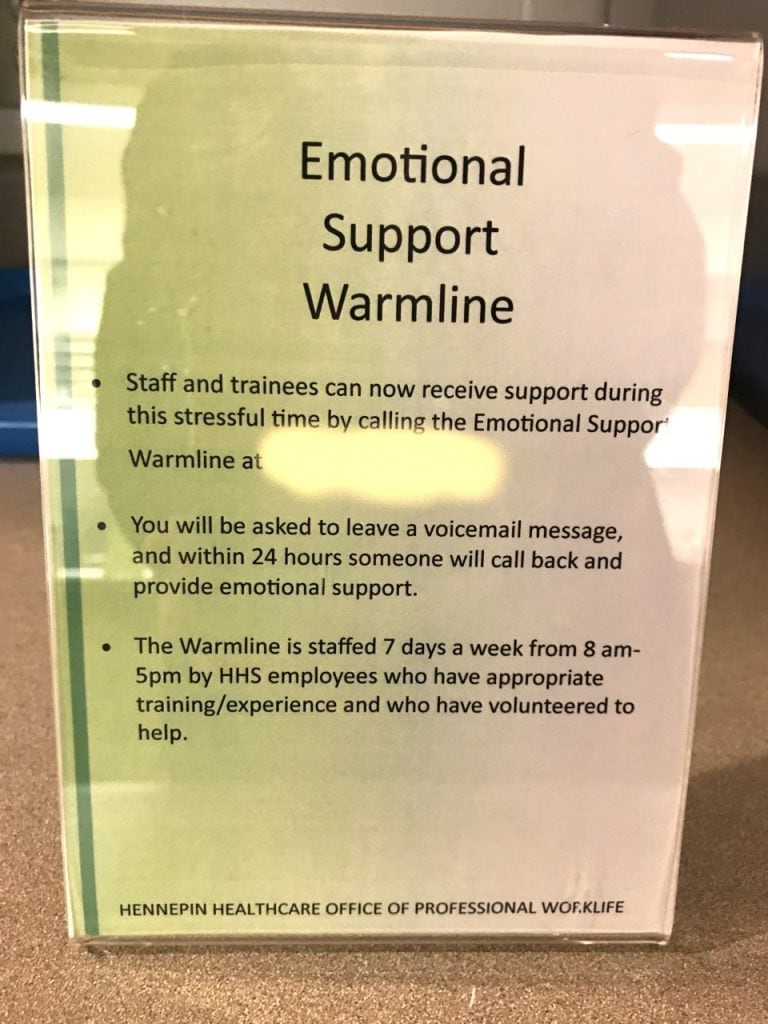
So at Hennepin Healthcare, we are offering small but real ways to support our colleagues. Just yesterday our Foundation provided food for the staff in the ICU and nursing units. To see our CEO Jennifer DeCubellis delivering 215 sandwiches to our staff is what we are all about.
Our Office of Provider Services provides healthy snacks in a quiet place of the hospital so that we can get away for just a minute. The manager in Labor & Delivery brought snacks for the nursing staff in that unit which must be present 24/7. Someone offered to cut hair. Our spiritual support team is made up of chaplains and spiritual healers who reach out to us every day. (I know, they reach out to me personally and for that I am grateful).
People in the community continue to offer masks and donations and words of support. From all of us, thank you for this.
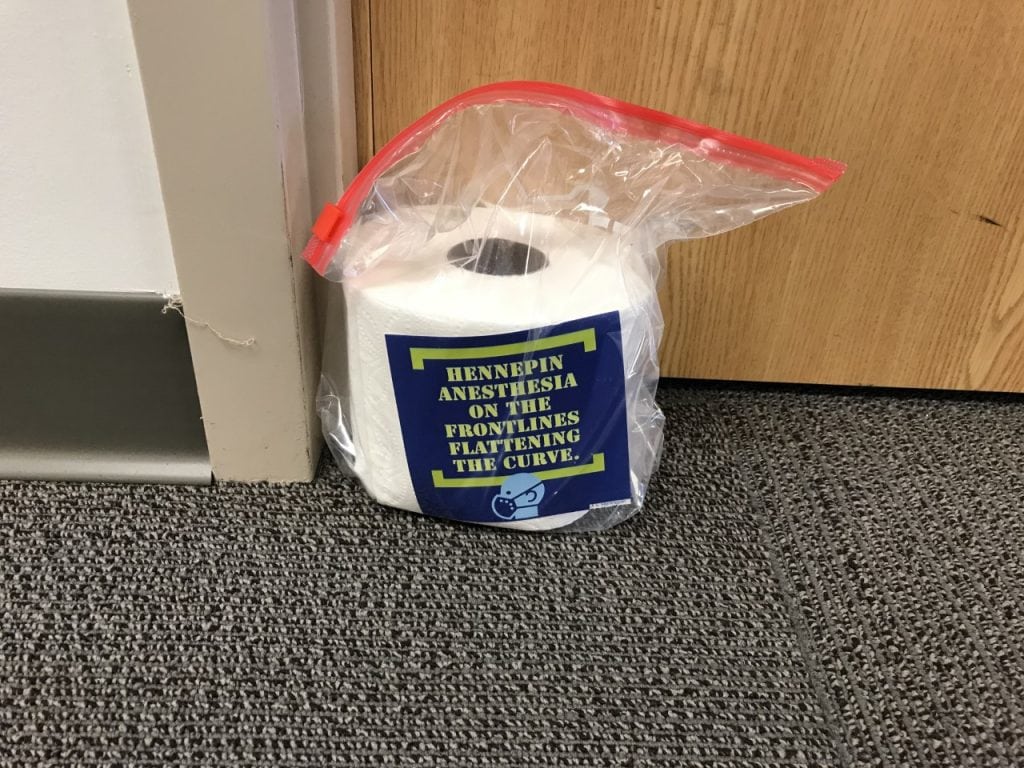
Our anesthesia department even did a secret dropoff of this coveted item to colleagues.
So we carry on, in what feels like the calm before the storm which is surely coming. Except even the calm isn’t so calm, because here in Minnesota we are gearing up for what our friends in New York are seeing now. I have a friend who is an Emergency Medicine doctor in Boston. Her strength is inspiring.
And so we take a collective deep breath and come back to the hospital and clinic the next day.
If you want to support the healthcare workers of Hennepin Healthcare, here are some ways:
- Write a word of thanks on our online thank-you page.
- Make a donation to the Hennepin Healthcare Foundation who will put it to good use in support of our staff. Just click the “Donate” button at the top. While on the site, you can learn much more about COVID-19, set up E-Visits, see a message from Jennifer DeCubellis our CEO, and much more.
- Perhaps most importantly, you can help by staying home. I mean really, stay home as much as you can. Consolidate trips to the grocery store so that you don’t go so often. Don’t congregate in groups ever, even when outside. What you do now will affect how our hospitals are able to manage in a few weeks.
So thank you!
David
Subscribe by e-mail to this blog if you want notifications of when a new post appears.
A doctor’s diary from a pandemic: Mental illness
Almost every day I walk through the patient care areas of our hospital at Hennepin Healthcare and lately I’ve been visiting the staff and patients in our 6 psychiatry units. Since I’m an internist, meaning I care for people with medical illness, I usual focus on patients on the internal medicine floors. But walking through the psychiatry units reminded me of the unique place people who experience mental illness are in.
At our hospital, just about 1 in 4 patients in the hospital is in a psychiatric unit with a mental health diagnosis. Possibly that is more than you realized previously. They are representative of all of us: rich and poor, young and old, urban and rural, you name it. Mental illness is a reality for all of our community. Furthermore, our mental health system is fragmented and historically we have not adequately provided a system robust enough to provide the care people need and deserve. So this pandemic presents unique challenges.
The current COVID-19 pandemic presents is hard enough for all of us. It produces anxiety in people who previously had not experienced such things. But for those who are experiencing mood disorders, psychoses, and other severe mental health conditions, it can be especially troubling. Coping with everyday life can be challenging in the best of times for people experiencing mental health issues. During this pandemic it can be crisis-provoking.
But the staff in the psychiatry units at Hennepin (and every other hospital) are skilled and dedicated to patients with mental illness. Here’s some insider info . . . the psychiatry units are not like regular hospital hallways that you may have in your head. They are more like a dorm at a college, with rooms down the halls around a common area when patients and staff co-mingle, eat together, watch TV together, and help each other heal. They have rooms for group therapy which are vital to the healing process. They have a kitchen-area where people have access to snacks. The nursing desks are centrally located which allows for lots of interaction.
All of this is challenging to do when coronavirus is on the mind of everybody. How do you do social distancing in that setting? How do the doctors and nurses and therapists promote healing when part of healing is socialization and group activities? How do you calm frazzled nerves when someone in a common area coughs or sneezes? How do you do all this when the length of hospitalization is measured in many days or even weeks?
Over the years I have become rather close to some of my colleagues in psychiatry and I appreciate the skill set of a psychiatry nurse or doctor so much more than I did a few years ago. So I write this post to honor those who care for people with mental illness and in support of those among us who are experiencing mental illness. During this pandemic – but really any time – I hope we all will check up on our friends and neighbors who may be struggling and to reach out to them by phone or from across the yard from a safe distance and offer a word of support.
Check out Minnesota NAMI for online courses and support.
For more good resources on mental illness, including COVID-19 information, check out the National Alliance on Mental Illness.
Follow me on Twitter if you wish @DrDavidHilden
A doctor’s diary from a pandemic: Social distancing in the hospital
So how exactly does one practice social distancing in a hospital?
We are struggling with how to be present for each other and for our patients all while keeping our distance. Those two priorities are sometimes – but not always – mutually exclusive. Being present is literally one of the tenets of person-centered care while keeping six feet apart is literally one of the tenets of social distancing.
Make no mistake, social distancing is necessary and we can do it. To prove it to you, check out our cafeteria at Hennepin Healthcare in this picture:
 Yup, we moved out all the tables to ensure we don’t get too close. Oh, we still stop and greet each other in the hallways, but do so from a reasonable 6 feet apart. Most meetings are by video or phone which is a mixed blessing: good becaues meetings are shorter and more to the point but bad because there is something lost when colleagues can’t see each other or laugh together or have a back-and-forth exchange of ideas. And coffee shops and gift shops are closed. The hallways in the areas of the hospital not directly involved in patient care seem oddly quiet.
Yup, we moved out all the tables to ensure we don’t get too close. Oh, we still stop and greet each other in the hallways, but do so from a reasonable 6 feet apart. Most meetings are by video or phone which is a mixed blessing: good becaues meetings are shorter and more to the point but bad because there is something lost when colleagues can’t see each other or laugh together or have a back-and-forth exchange of ideas. And coffee shops and gift shops are closed. The hallways in the areas of the hospital not directly involved in patient care seem oddly quiet.
So like you at home, we do our best to be present while being far apart.
But what about our patients? The hallways on the patient care floors are still buzzing with the usual activities of patient care. But with patients, how does one practice social distancing? This one is way harder. Masks make it harder to read the face of people, for instance. It is hard enough to give hard and potentially scary news to a patient but even harder when you are wearing a surgical mask and gown and standing across the room.
How about human touch, that most basic part of being a doctor or nurse? If I’m not going to gain any meaningul knowledge that will help you by listening to your chest with my stethoscope, I probably shouldn’t take the risk and I should not touch you at all.
Perhaps hardest of all and the aspect of this COVID-19 pandemic that I can’t get my head and heart around is the restrictions on visitors when someone is critically ill. Our hospital has rightfully limited all visitors to just one at at time to prevent transmission of COVID-19. It is absolutely the right thing to do to protect as many patients and visitors and staff as possible. But some hospitals in the US have limited visitors to zero and we may get to that point as well. We have some extreme end-of-life compassionate care exceptions, but even those exceptions will be less frequent if this pandemic worsens.
There was a piece in the New York Times, called “I’m on the Front Lines. I Have No Plans for This.” It is written by a critical care doctor, Dr. Daniela Lamas, at Brigham and Women’s Hospital in Boston. This is a US hospital. I have friends who are doctors there. This isn’t some far off hospital in another country. This is in one of our country’s premier hospitals. I encourage you to read what Dr. Lamas writes about the real possibility of a “medical solitary confinement” in which patients in COVID-19 wards may be dying alone.
I doubt I’ll ever truly come to accept the possibility that people will be alone while critically ill. I never want to see that. So that is why we practice, and you should practice, social distancing.
Thanks for checking in with this free-form, stream-of-consciousness diary from a pandemic. I’ll write more in a couple days.

