Back in April I posted about medical science and what I had learned at my latest continuing education conference (the American College of Physicians conference in San Diego). Go ahead and re-read that post to get my thoughts on how to approach medical science. I had said that I’d be doing future posts about some of what I learned at doctor school in San Diego. The first of those was a look at Clostridium difficile (C. diff) infections. Now I’m tackling Lyme disease, much at my own peril since there is raging controversy about this one – at least with some folks.
Back in April I posted about medical science and what I had learned at my latest continuing education conference (the American College of Physicians conference in San Diego). Go ahead and re-read that post to get my thoughts on how to approach medical science. I had said that I’d be doing future posts about some of what I learned at doctor school in San Diego. The first of those was a look at Clostridium difficile (C. diff) infections. Now I’m tackling Lyme disease, much at my own peril since there is raging controversy about this one – at least with some folks.
Here’s what you’ll find if you read on:
- Lyme disease basics.
- Acute Lyme disease.
- Post Lyme Disease Syndrome, which some call “chronic Lyme disease.”
Fasten your seat belts, here we go . . .
First, the basics

Photo: Magicpiano via Wikimedia Commons
Let’s start with terminology – it is Lyme disease, not Lyme’s disease. It is named after the town of Lyme, Connecticut, which is where the first cases were found in the 1970s. In the picture is bucolic Lyme, which to me looks a lot like Minnesota. Makes you want to take a hike. But there’s a hidden danger in this picture – you can practically see the ticks in there. Or at least imagine them. Or feel them crawling up your leg. Ew.
The culprit in Lyme disease is a spirochete, which is a corkscrew-shaped bacteria, called Borrelia burgdorferi, which is in turn named after Willy Burgdorfer. A native of Switzerland who later settled in Hamilton, Montana, he was a self-proclaimed “tick surgeon” who isolated the bacteria responsible for the curious cases of rashes, fatigue, and joint pain being seen at oddly high rates in Lyme, Connecticut. He was honored by having the bug named after him. We owe a lot to nerdy guys like Willy Burgdorfer who spent hours and hours literally dissecting teeny ticks. Cool. He died just a couple years ago and you can read about him the New York Times.
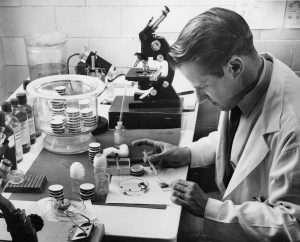
Willy Burgdorfer. Public domain photo by Nicholas J. Kramis
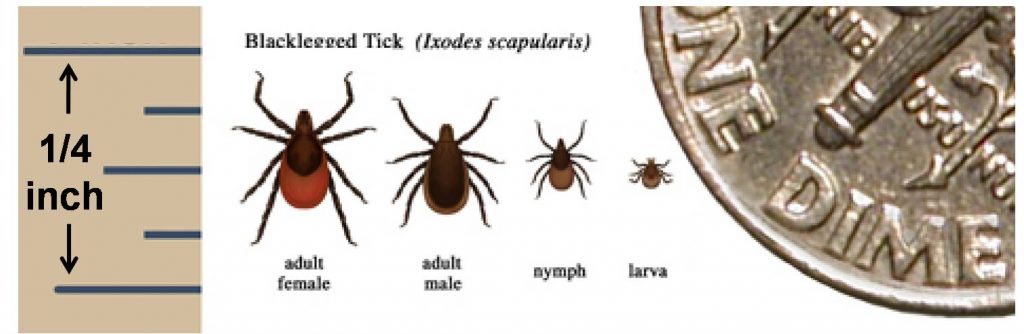
The bug in question lives in black-legged ticks (scientific name Ixodes scapularis). These ticks live on mice, other rodents and bigger mammals, such as deer. Hence the previous name deer ticks. In my own state of Minnesota, they are all over the place in large numbers especially from the Twin Cities north and eastward. My friends in the St. Croix valley of northeastern Wisconsin are in tick ground zero.
Check out this map. I’m looking at you, Minnesota. And wowie check out the Northeast (where it all began).
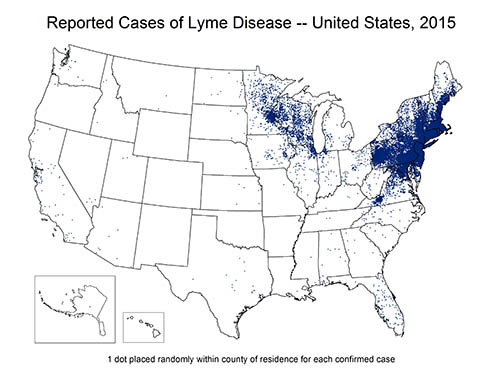
Source: CDC
Getting Lyme disease
You get Lyme disease when an infected black-legged tick gets on you, attaches itself, and stays there for a couple days thus transmitting the bacteria to your blood. It is usually the immature nymph stages that get you since they are so small you can’t see ’em. You can get Lyme from adult ticks as well, but since adults are just a little bigger, you are more likely to spot them crawling on you and flick them off. Nymphs are smaller and can attach to you without you knowing it. They are only the size of poppy seeds!
Note that the tick has to be attached to your skin – at least for 36 hours – for it to transmit the disease. So if the tick is crawling on you you’re in the clear. Just flick it off!
The ticks don’t just fall from the sky. In fact, they are more likely to be in the bushes and grasses on the ground where they can crawl up your legs. This is why hunters dressing deer are at risk as they are down at ground level. Campers and hikers, too, as they venture into the tall grasses with shorts on. They can also get on your dog who is enthusiastically romping through the woods. From your dog they can hop onto you.
Look at the picture above and note how small these bugs are, especially the nymph stage. If it’s one of those big wood ticks, as gross as that may be, you’re not going to get Lyme from it.
Best to wear long pants and socks and use a bug repellent.
This time of year (late May) is when the invasion really gets into high gear here in much of the United States. So we are in high tick season, folks!
Acute Lyme disease

Public domain photo Hannah Garrison
Lyme Disease is the most common vector-borne disease in the United States. In this case, the tick is called a vector, or carrier, of the disease. Distinguish that from human-human transmission of a disease. The hallmark is the erythema migrans rash, which is a dead giveaway for Lyme. Problem is, not everybody gets the rash and even those that do get it may not notice it. Most experts put the incidence of the rash at well over 50% and perhaps as high 80%. Since this is tough to measure – especially when people may not even know they have a rash – some people think that the rash isn’t nearly so common as that. So you can totally get Lyme Disease without a rash. Lots of people do.
In addition to the rash, symptoms of acute Lyme Disease may include:
- Fever
- Chills
- Joint aches and pains
- Fatigue
- Swollen lymph nodes
- Muscle aches
- Headache
Later on, if untreated, people can get:
- Severe headaches
- More of the rash on other parts of body
- Severe arthritis (joint pain)
- Facial paralysis
- Heart rhythm problems
- Inflammation of the central nervous system
- Severe fatigue and muscle pain
- Memory problems
- And other non-specific pains, numbness, dizziness . . .
- In other words, it can be serious.
Treatment of Lyme disease

Close up of Borrelia burgdorferi
The best science we have available says that the Lyme disease bacteria can be effectively treated with a relatively short course of the appropriate antibiotic. I put that sentence in red because there are many who don’t agree with that and believe that the treatment needs to be longer. However, a review of the highest-quality evidence supports the current recommendations that just a few weeks of the right antibiotic is sufficient. In some cases, the recommendations call for extending the duration of antibiotics.
I’m quite sure there are people reading this that disagree with that previous paragraph and I respect that. But I work with Infectious Disease doctors every day whom I respect a great deal and who have nothing to gain from any particular viewpoint. This is the overwhelming conclusion of the experts and I’m sticking with their wisdom.
Chronic Lyme disease. Is there such a thing?
I’ll grant that there is a little controversy about how long to treat acute Lyme disease (although not among anyone I know who practices Infectious Diseases). But this next part is not a little controversial. It is really, really, controversial for some. Here goes . . .
It is true that some people, after having been diagnosed with and treated for Lyme disease, continue to feel unwell. Sometimes the symptoms go on for months. Or even years. This is true and most everybody I know acknowledges this reality.
The controversy is about why this occurs. Most scientists and clinicians have concluded that there is a Post-Lyme Disease Syndrome (PLDS) in which some poorly understood mechanism continues to cause aches, pains, fatigue, headache – all the stuff that makes people truly miserable. The cause is admittedly not known but leading hypotheses hold that it is immune system and tissue damage that is slow to heal in some people.
What is widely accepted to NOT BE THE CASE is that there is an ongoing infection with the Borrelia burgdorferi bacteria that is causing the symptoms.
OK, I put that sentence RED AND BOLD because there are many people who strongly dispute that conclusion. They feel that there is ongoing infection with the bug and that long-term antibiotics (sometimes for months or even years) are needed to eradicate it. They refer to that as chronic Lyme disease.
However, the research about this issue is convincing to most people I know – there is no ongoing active infection so long-term antibiotics are not helpful and perhaps harmful. That being said, there are chronic Lyme disease support groups, foundations, and professional organizations who are vocal in their advocacy for CLD. In my opinion, we should listen to these folks since I have not yet met the person who knows the absolute truth about anything. But I wish we had a collaborative and – well, nicer – working relationship with both sides of the Lyme controversy. The reality is that we don’t.
What is wrong with long-term antibiotic use?
There are real downsides to long-term antibiotic use. Here are three of them:
- Breeds resistance to antibiotics which is a huge public health concern for our society.
- Side effects of antibiotics are real and can be very serious, even life-threatening. Things like diarrheal illness up to and including C diff (see my previous post), allergic reactions, secondary infections. People have died from long-term antibiotics while being treated for so-called chronic Lyme disease.
- Gives false hope based on poor quality research. This is a disservice to people.
There actually are high-quality studies that show that people who are being treated for so-called chronic Lyme disease respond just as well to placebo as they do to antibiotics. You don’t even have to administer a real drug since the success rate is about the same. It may take a long time but most people do get better in the long run and without long-term antibiotics.
I imagine I’ll get nasty comments about this. But I believe that it is the doctor’s duty to give advice based on the best-available science while simultaneously and kindly listening to and validating the real illness that people experience. Far from abandoning people with post-Lyme symptoms, we should listen and acknowledge those symptoms. Then we should doggedly work with those patients to help relieve their misery. We can’t do this by promoting unsupported methods and giving misleading or even false information.
I’ll leave you with a pic of the azalea shrub in my front yard. It burst into color this week and it just must be shared. Here it is:

David
Stay in touch! Follow me on Twitter @DrDavidHilden and subscribe by e-mail below.