Think men and women are just the same? No, I didn’t think so. But when it comes to heart disease, much of what the medical community talks about is focused on men’s heart health. So on the Healthy Matters radio broadcast last Sunday, we focused on women’s heart health.
I was joined in the WCCO studios by two women whose careers are focused on caring for hearts. They are Dr. Michelle Carlson, a cardiologist, and Jill Jordan, a Certified Physician Assistant with clinical practice in Cardiology. Not only are these two really knowledgeable about cardiology in general, they are particularly tuned into the health of women. Not only that, they do cool work with cancer and heart disease. And I can personally vouch that they are approachable providers with a good listening ear and wise advice for their patients.
Three things you can do to learn more:
- Listen to the podcast of the Women’s Heart Health show by clicking the logo here. It is Healthy Mattes Show #482, April 8, 2018
- Click Dr. Carlson and Jill Jordan’s pictures here for their bio and contact information, or go to the Heart Center at Hennepin Healthcare to learn more and including info on making appointments.
- Read on for brief and informative answers to listener questions that we did not have time for on the radio broadcast. Heart attack, jaw pain, ischemia, family history, varicose veins, valves, exercise, diet, yoga. It’s all here! The responses are directly from Dr. Carlson and Jill Jordan. Don’t miss the last question (scroll down!) about heart disease and cancer. Pictures and links, too!
Women’s heart health
Why is it important to talk specifically about women’s heart health?
Dr. Carlson: Everyone has a heart, but we’ve spend a lot of time and energy researching men’s heart disease and treatments and raising awareness of the risk of heart disease for men without putting the same focus on women. I think it’s important to think about how their symptoms might be different, how they might respond to medications differently (for example, a woman having regular menses is at higher risk for bleeding with some of the medications we use), and how various hormonal changes at different times of life (like pregnancy and menopause) can affect the heart.
A few questions about coronary artery disease and heart attack
What warning symptoms of a heart attack should prompt me to call 911?
Jill Jordan: The American Heart Association recommends calling 911 if you experience chest discomfort lasting more than a few minutes, or that goes away and comes back, pain or discomfort in one or both arms, the back, neck, jaw or stomach, concerning shortness of breath, with or without chest pain, a cold sweat, nausea or very bad lightheadedness. Obviously, a few of these symptoms might come now and then to a low degree. When the symptoms are debilitating or very atypical for you, you should always call 911. Learn more from the AHA here.
Can jaw pain be a sign of heart problems?
Jill Jordan: Acute pain in the jaw or chest pain that radiates up to the neck and jaw can be a sign of heart disease. This is one of those “atypical” symptoms that women tend to have more than men, although men can have jaw pain with heart disease as well. If you currently have jaw pain that is attributed to TMJ or other issues, this does not indicate that you will have trouble in your heart down the road.
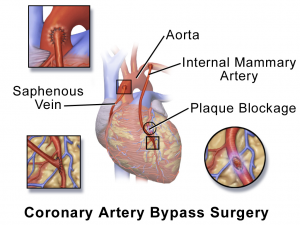
I am 8 yrs post coronary bypass surgery x 3. At age 73 what is the expectancy of the bypasses staying open?
Dr. Carlson: It depends on the type of bypass used. The LIMA, or left internal mammary artery, is often used to bypass the main artery on the front of the heart. This often stays open for the rest of your life. Other bypass grafts are usually required as well. The most common are vein grafts from the legs. Historically, when we look at patients overall about 50% of vein grafts are open 10 years after the surgery. Less often, a radial artery graft is used. This appears to stay open longer than vein grafts.
I am 64 and last year my doctor told me I have coronary heart disease. I am on cholesterol meds. What else can I do to live into old age?
Jill Jordan: First of all, if you smoke, QUIT! You can find help through QuitPlan or through the Smoking Cessation Clinic at Hennepin Healthcare. Other things you can do to prevent the progression of coronary heart disease is controlling diabetes, keeping your blood pressure under control, be physically active every day, follow a heart healthy diet, aim for a healthy weight, reduce stress, and limit alcohol.
I am a 55 year old female. Heart disease runs in my dad’s family. He had quadruple bypass in his 50s. What should I watch for?
Jill Jordan: It is great that you’re being proactive and thinking of ways to watch your own health! It is always important to watch for decreases in your functional status. If you used to be able to go up 3 flights of stairs and now have to rest after one, or if you used to walk 1 mile but now get short of breath after a few breaths, it is important to talk to your doctor. Focus on prevention for now (diet, exercise, limiting alcohol, reducing stress) and keep a close relationship with your physician, so they can pick up on these changes.
What the heck is ischemia?
What is ischemia? Prognosis and treatment? 66 yr old woman.
Dr. Carlson: “Ischemia” means that your heart muscle isn’t getting enough blood flow, usually because of a blockage in a heart artery. There is a whole range of what ischemia can look like, from chronic stable angina (where someone has regular chest pain that is coming from the heart) all the way to a big bad heart attack that requires a call to 911. The prognosis and treatment depends on the kind of ischemia that you are experiencing, but will probably involve some combination of medications as well as the possibility of an angiogram, depending on your exact situation. I encourage you to talk to your doctor about this question.
Something completely different: varicose veins
What role do varicose veins have in heart disease?
Jill Jordan: Veins are vessels that carry blood back to the heart and lungs to be oxygenated. A varicose vein is an enlarged or damaged vein that allows blood to flow backwards. While veins have a role in circulation, and varicose veins may affect circulation, there isn’t necessarily a connection between varicose veins and heart problems.
Your heart is just fancy plumbing. Valves and all.
I have been told, from a CT, that I have some plaque, no bulging, in my aortic valve. What is done for that, or does it go away at all
Dr. Carlson: Unfortunately, we don’t have any treatment for plaque or calcification on the aortic valve at this time. Unlike plaque in the heart arteries, it doesn’t improve with statin therapy. It’s very normal to see calcification on the aortic valve as we age. Sometime, however, it can be associated with narrowing or leakage of the valve. You should talk to your doctor to make sure this isn’t the case for you.
Some preventive cardiology: exercise, yoga, alcohol
Tell us more about the role of exercise in women’s heart health–
Jill Jordan: The best thing you can do is get moving in a way that brings you joy! Jogging every day and hating it isn’t a great long-term plan. There are so many ways to move – swimming, biking, volleyball, walking, tennis, dancing and more. Pick what works for you and your lifestyle. The American Heart Association recommends 30 minutes of moderate-intensity aerobic activity (that means heart pumping!) daily, or 150 minutes per week. If your aim is to lower your blood pressure or cholesterol, aim for an average of 40 minutes of moderate-vigorous intensity aerobic activity 3-4 times per week. And remember, SOMETHING is better than nothing. Even 5-10 minutes of walking a day can make a difference in your overall heart health.
Is yoga good for my heart?
Jill Jordan: You betcha! There are different types of yoga—some are based on stretching and strengthening, others are devoted to meditation and relaxation. The good news is that all kinds are good for your heart health! Practicing yoga, as part of an overall healthy lifestyle, can help lower blood pressure, increase lung capacity, improve balance, boost circulation, tone muscles, reduce stress and improve your sense of well-being. While I highly recommend adding yoga to your daily or weekly routine, know that unless it is a flowing yoga that gets your heart gets pumping, it doesn’t count towards your 150 minutes-per-week of recommended moderate activity!
What about alcohol? I hear red wine is good for my heart.
Jill Jordan: Over the past several decades, many studies have been published in science journals about how drinking alcohol may be associated with reduced mortality due to heart disease in some populations. Hypotheses on why this is includes the role of antioxidants, an increase in HDL (“happy/healthy”) cholesterol or anti-clotting properties. While the strongest support is for the rise in HDL, you can raise your HDL in other ways, including exercise. The American Heart Association does not recommend drinking wine or other forms of alcohol to gain these potential benefits. If you do drink, to be heart healthy limit yourself to 1 drink per day for women and 2 drinks per day for men. And no, you can’t save them all up and drink 7-14 drinks on the weekend! Read lots more about cholesterol from the American Heart Association here.
What is a cardiac arrest?
My 82 year-old mother suffered a “cardiac arrest” this past Friday and did not survive. How does a “cardiac arrest” differ from a “heart attack”?
(Note from Dr. Hilden: listeners to the live radio broadcast or on the podcast will note that we answered this question on the radio, but it seemed important enough to include here as well).
Dr. Carlson: A “cardiac arrest” means the heart stops working, which can be caused by many things. A “heart attack” or “myocardial infarction” is a sudden blockage in a heart artery. Sometimes it causes pain first and gives the patient time to get help, but if the blockage is severe enough, it can cause a cardiac arrest. So, some heart attacks (but not all) can lead to a cardiac arrest, and some cardiac arrests (but not all) are caused by heart attacks.
A broken heart?
What is the difference between a heart attack and a “heart break”? I’m a female (46) and I have some pain, but I’m also grieving the loss of my mother.
Dr. Carlson: A heart attack is usually caused by a blockage in the heart arteries, usually from a combination of ruptured cholesterol plaque and platelets. We diagnose a heart attack based on symptoms, the electrocardiogram (EKG), and heart enzymes in the blood. Sometimes a patient comes in with pain, EKG changes, and heart enzyme levels that are consistent with a heart attack, but when we look directly at their heart arteries with an angiogram there is no blockage. This can sometimes be caused by “stress cardiomyopathy,” also called “tako-tsubo cardiomyopathy” or “broken heart syndrome,” where the heart becomes very stressed by an emotional or physical event and temporarily stops working normally. The good news is that the heart is able to recover from stress cardiomyopathy and go back to working normally, usually after a few weeks.
Note from Dr. Hilden: what does broken heart cardiomyopathy have to do with this critter? Click the picture to find out.
Cancer and heart disease: caring for the whole person
What heart problems can occur for women getting treatment for cancer? Chemotherapy? Radiation?
Dr. Carlson: Different treatments for cancer have different effects on the heart. Some chemotherapies that are used to treat breast cancer can weaken the heart muscle in some women, and can even cause heart failure, which is when you start to have symptoms like weakness and shortness of breath because the heart muscle is so weak. Other chemotherapies can increase the risk of a heart attack or of having an abnormal heart rhythm (again, not all people who receive the chemotherapy will have these problems—in fact, most do not). Radiation to the chest can sometimes cause problems in the heart arteries, the valves, the sack that surrounds the heart, or in the heart muscle itself. This usually occurs a decade or more after the radiation treatment is completed. In cardio-oncology, we try to identify those who are at increased risk for a heart problem and do what we can to decrease that risk, including things like controlling high cholesterol and high blood pressure. Your oncologist (cancer doctor) is the best person to talk to about the risks of cancer treatment for you, and she or he can help decide if it’s right for you to see a cardiologist before, during, or your cancer treatments.
A note from Dr. Hilden: Dr. Carlson and Jill Jordan are your “go-to” providers for heart disease. And if you have cancer, that’s even more true. In the Twin Cities, you can see either of them by going to the Hennepin Heart Center or call 612-873-6963 and ask to make an appointment with them. If you see them in the clinic, tell ’em I sent you!
Thanks so much to Jill Jordan and Dr. Michelle Carlson. Two great colleagues! Two great providers!
Please subscribe by e-mail to MyHealthyMatters.org. It’s easy and don’t worry – I won’t send a bunch of mass e-mails to you! And I really recommend you listen to the podcast of our women’s heart show – use the link at the top of this post.
-David
Twitter @DrDavidHilden