Hey, everybody. Check out this fact: about 16 million people in the United States will experience an episode of depression every year. That’s about 7% of the population. By some estimates, depression is in the top 3 causes of disability (source: World Health Organization).
To help us learn a bit more about this condition, I asked my colleague Dr. Eduardo Colón to be my in-studio guest on last Sunday’s Healthy Matters broadcast. It was a great show! Dr. Colón is the Chief of Psychiatry at HCMC and he has been on the show a few times over the years. This is terrific since you will not find a wiser and kinder psychiatrist than he. I really encourage you to listen to the podcast so you can hear Dr. Colón explain things much better than I can in this written form.
You can learn more about Dr. Colón from this Minneapolis Star Tribune article which appeared shortly after he was named Chief of Psychiatry. He gives an insider perspective on mental health care in our community that is worth a read.
I’ll use this blog post as a written companion of sorts for the audio podcast of that radio show. I’ll try to encapsulate a few topics from the show and include some links for more information.
First of all, download the audio podcast here to listen to whenever you want. Once at the podcast site, select Healthy Matters show #475, February 11, 2018).
A wealth of information on depression
Here’s what Dr. Colón covered on the show, and you can click the links to jump to specific topics that interest you.
- How common is depression?
- How is depression diagnosed?
- What is seasonal affective disorder?
- What are treatments for depression?
- Brief comments about suicide. Includes crucial link to suicide assistance.
- Can depression be treated by primary care doctors or is a psychiatrist needed?
- The stigmatization of depression. This section includes a link to a powerful short essay by a medical student that I highly recommend you read.
- Depression and stressors in relationships in our political environment.
- Social media and depression.
- How to distinguish normal grief from clinical depression.
- Is there a hereditary risk for depression?
- Is there a link between acne medications and depression?
- How to get help for people in your life who may have depression. Important link to NAMI in this section.
- Does having money protect you from depression?
- Can you ever stop depression medications? If a maximum dose of an anti-depressant doesn’t work, what then?
- Is there a link between depression and heart problems?
Depression explained by Dr. Eduardo Colón
How common is depression (Audio podcast time: 4:36)
Depression is really common. As many as 7-8% of the population in the US will experience an episode of depression at some point in life. Some people have just a single episode but many have repeating episodes. For more detailed statistics on depression (including differences among age, sex, and racial groups), check out this reliable site from the National Institutes of Health.
How is depression diagnosed? (5:22)
Dr. Colón points out that the definition of clinical depression (“Major Depressive Disorder” in medical terms) has evolved over time. Is the word “depression” even overused a bit? One guy called it a “wimp” of a word since it has lost much of its meaning in our common language. But there are some criteria for depression:
- Loss of interest or loss of pleasure in all activities
- Change in appetite or weight
- Sleep disturbances
- Feeling agitated or feeling slowed down
- Fatigue
- Feelings of low self-worth, guilt or shortcomings
- Difficulty concentrating or making decisions
- Suicidal thoughts or intentions
If these symptoms are lasting two weeks or more, depression may be diagnosed. For much more from a terrific organization, go to the National Alliance of Mental Illness site on depression. Here’s also a great one-minute video from NAMI that I recommend:
Seasonal affective disorder (7:50)
Some people get depressive episodes, usually in the fall when the days are shortening. And it turns out that there is a pattern – more likely in a) people who live in northern latitudes, b) younger people, and c) women. More from NAMI here.
Treatments for depression (10:26)
Many of us think only of medications for treating depression. But Dr. Colón reminds us that there are a range of treatments, starting with strategies that people can do on their own: exercise, diet, yoga, and so forth. There are also a variety of psychotherapy (cognitive behavioral therapy and interpersonal therapies) for mild-moderate depression that have been shown to be as effective as medications. When the depression gets to be more moderate to severe, all the previous interventions are helpful but this is where medications are really needed. Mostly recently, augmentation with a 2nd medication to the anti-depressant has been shown to be beneficial to many. Electroconvulsive therapy (ECT) is very effective for severe depression, especially when accompanied by psychotic features. The bottom line: there are many treatments for depression that can help.
Suicide and depression (12:45)
Suicide is such an important topic that it requires its own discussion. But for our purposes here, I want to give one potentially lifesaving link: National Suicide Prevention Hotline. Clink the link or call 1-800-273-8255. Did you know that if you put “suicide” in Google it will bring up this link? These are important, potentially life-saving resources, 24 hours a day, 7 days a week.
Can depression be treated by a primary care doctor? (14:04)
There are not enough psychiatrists in the world to help everybody with depression. But that doesn’t mean you can’t get help. The first stop for people who may have depression is often their primary care physician who can make the diagnosis and start treatment.
If nothing else, your primary clinic should be able to screen you for depression. To do this, they simply need to ask you two questions:
Over the past two weeks, how often have you been bothered by any of the following problems:
- Little pleasure or interest in doing things? (this is the anhedonia question)
- Feeling down, depressed, or hopeless? (the depressed mood question)
Both are answered from 0 to 3 (0 = Not at all and 3 = Nearly every day). This isn’t a full diagnostic test, but it does remarkably well at helping your clinic provider decide when to look further. A score of 3 or more when the two questions are added together suggests that further evaluation for depression is warranted. For more detail on the PHQ-2 screening tool, click here.
Stigma and depression (15:14)
One of the Healthy Matters listeners questioned whether letting your insurance company know that you are being seen for depression is a good idea. Brings up the old issue of stigmatization of mental health. It’s a legitimate concern but hopefully, as Dr. Colón said, a concern that we as a society are moving beyond. Are we moving beyond it? Probably not nearly as much as we should. We don’t say a person with heart failure is weak in character. We don’t tell a person with asthma to just “suck it up” and be stronger. But we sometimes do with someone with depression.
I encourage you to read an essay that came out just this week. In it, Rachael Gupta, who is a medical student, bravely discusses her own journey with depression. She says,
“Depression is not weakness, though depression is a disease that may make you feel weak.”
Please read her essay from JAMA here. Should be required reading for all of us.
Families stressed out over politics – can you relate? (17:25)
Listen to the audio podcast for a discussion about the stress within families and friends due to our polarized political environment. Dr. Colón has wise advice on the subject.
Social media and our mental health (24:23)
While social media can help keep us connected in some cool new ways, it can also lead to social isolation. I have a feeling we are going to hear much more in the coming years about the effects on our mood, our individual mental health, and our societal connectedness. Do you have thoughts on this? Leave a comment in the below!
When does normal grief become a concern? (26:09)
Such an important question: when we suffer a big loss like the death of a loved one, it is completely normal to feel completely in grief. But how do we know when that normal grieving process becomes abnormal. Dr. Colón stressed that trajectory of grief is important. In other words, gradually, a grieving person should be re-connecting with others, re-engaging with his or her community, and resuming pleasurable activities. If this is not occurring after many months, maybe more help is needed.
I’ll direct you to my own healthcare organization’s Spiritual Care Department, who has assembled a good list of resources for specific grieving situations. Maybe they can help you in the more than dozen links to good grief resources.
Is there a genetic component to depression? (28:10)
The short answer is . . . yes, there is a genetic component. Depression may be more likely in someone who has a history of depression in the family. We also know of other factors that put people at higher risk, including childhood neglect, trauma, abuse, loss, brain injuries, and some medical illness.
Depression and acne medications (29:05)
I haven’t thought of this much lately but there used to be a concern that acne medications may put adolescents at risk for depression. Dr. Colón noted that we are somewhat less concerned with that in recent years, but he also noted that adolescents with severe acne may have self-esteem and social marginalization issues and that in turn can manifest as mood problems like depression.
How to help family and friends with depression (30:39)
This is a big question: how do we help those close to us who may have depression? How do we support each other and support ourselves? The best resource I know for resources to assist is from the National Alliance on Mental Illness (NAMI). As promised on the air, here is the link to the NAMI website. It is a great starting place for resources to help patients, families, and anybody interested in learning more.
Does having money protect against depression? (33:51)
In a word, no. Money may buy convenience, but people at all income levels can get depression.
When can I stop anti-depressants if I am no longer having problems? What about if I’m on the maximum dose of anti-depressants and still having problems? (35:33)
Listeners raised these interesting questions. They are big topics and, of course, we can’t give specific medical advice over the radio! But there are some basic principles:
- People who have 3 or more depressive episodes in their life should probably be on medications indefinitely, since 95% of them will have another episode in the future.
- If considering stopping your anti-depressant, best to do it under the close watch of your doctor or other provider. Tapering off the medication slowly and watching for symptoms is the way to go.
- People should probably stay on anti-depressants for a good year or so following an episode of depression.
- As always, other interventions (the lifestyle ones we mentioned above, therapies, etc) should also be used.
Depression and heart problems (37:43)
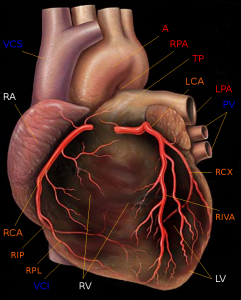
By Patrick J. Lynch (1999), modified by Christian 2003 (Yale University – School of medicine) via Wikimedia Commons
The last minute of the radio show involved an intriguing question: does depression have any connection with heart attacks? Well, we’re not sure, says Dr. Colón. But there are some credible possibilities. Perhaps a person with depression has a different stress response, which in turn makes the vascular linings and clotting mechanisms of the heart function differently – perhaps leading to more heart disease. Fascinating twist on the connection between mental and physical health. Here’s an informative site from Johns Hopkins on the relationship between heart disease and depression.
I want to thank Dr. Eduardo Colón for lending his expertise to an information-packed show. He breaks down mental illness so skillfully. Thanks to you, as well, for reading the blog. Subscribe below by e-mail if you wish. (No marketing or spam will come your way, just a notice when a new post comes out a few times per month).
David




