 October was Breast Cancer Awareness Month and I welcomed two outstanding experts to the WCCO studios for the live broadcast of Healthy Matters. We focused on the common screening test – the mammogram – and tried to answer your questions about this well-known but still sorta mysterious test that women (and a few men) get all the time.
October was Breast Cancer Awareness Month and I welcomed two outstanding experts to the WCCO studios for the live broadcast of Healthy Matters. We focused on the common screening test – the mammogram – and tried to answer your questions about this well-known but still sorta mysterious test that women (and a few men) get all the time.
To help me, I turned to repeat radio guest and my friend Dr. Tony Severt. He is the Assistant Chief of Radiology at HCMC (the mother-ship where I work) and is a expert in women’s imaging, including mammograms and other breast imaging (like ultrasound and MRI).
As an aside, there is a bit of wisdom that some doctors heed . . . that it is always good for us non-radiologists to have a “go-to” radiologist to help us when we need advice on the best imaging to order or how to interpret the imaging that we have. Dr. Severt is my “go-to” guy! He’s smart, really understands the patient perspective, and he is kind and willing to help. So I dragged him down to the studio last Sunday morning.
But Dr. Severt is not the one who actually performs the mammogram. That job goes to mammogram technologists who are highly skilled, patient-focused, and dedicated professionals. These women (yes, the mammogram techs are all women as it should be) are supervised at HCMC by Leah Hahn. Leah joined us in the studio to give the first-hand perspective of one who knows her stuff about mammograms. For more about mammograms, click the HCMC radiology page here. And for an advance look at Minnesota’s newest and finest breast care center, scroll to the bottom of this post!
As always, the best way to catch up on a past show is by listening to the podcast. Click this logo to reach the main podcast page, then select Healthy Matters show #460, October 29, 2017.
The problem, as usual with a live radio broadcast, is that we never get to all the questions that people call and text in to us. So the rest of this post is simply a Q&A. I’m using the text questions that listeners sent and have asked Dr. Severt and Leah to give their responses. Here they are . . .
Q: My doctor hasn’t done a breast exam in 15 years. He said it was not necessary.
Dr. Severt: The American College of Radiology stance on this is “It is not wrong for a doctor to examine the breasts, but it is unlikely to be of benefit to the woman.” Clinical breast exam – or CBE – will detect something around 3 cancers per 10,000 women examined, and will lead to many more false positives per cancer than mammography. If you are getting regular mammograms, your doctor is correct. A breast exam does not add value.
Q: I was diagnosed with breast cancer at age 40 . . . Why do certain doctors say let’s “watch” the lump on your breast to see if there will be a change rather than doing a biopsy?

Dr. Tony Severt
Dr. Severt: It’s not just certain doctors who do this. All mammographers do this using the accepted algorithm in certain situations. When we find something that is really a finding, but we think is probably benign, we use that category. The lesion has to have a likelihood of malignancy in the 0.3-1.7% range. That means it looks very benign, but since it’s new we will keep an eye on it. Watching for 6 months can eliminate many unnecessary biopsy procedures. This is part of the mammography algorithm, so if a doctor is doing things right, he or she will use this category in some lesions. In my practice, I ask women to come back before the 6 months if there is a change in the lesion or if they become too worried to wait.
Q: My mom had breast cancer in her 70s. What does that mean for me at the age of 57.
Dr. Severt: Your risk of developing breast cancer is increased compared to someone in your exact same situation who does not have that family history. This risk might not end up being much above the relative population risk depending upon all of the other risk factors, but it is higher than it would be without that family history. You can ask your doctor about a breast cancer risk analysis. If you come to HCMC for your mammogram and give that family history, our technologist will help you fill out a questionnaire to help determine your lifetime risk.
Q: Does someone with a history of fibroadenomas and fibrocystic benign breast disease have a greater risk of developing breast cancer?
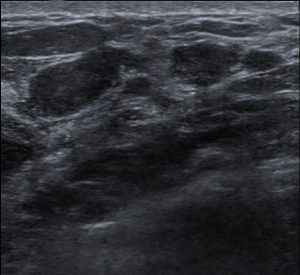
Ultrasound of breast fibroadenomas By © Nevit Dilmen, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=19738585
Dr. Severt: Fibroadenoma does not carry any increased risk of breast cancer. Fibrocystic breasts are, in general, dense breasts. There may be an increased risk of breast cancer associated with dense breasts, those studies we have on this topic are not definitive. However, we do know for sure that dense breast tissue makes it more difficult to diagnose cancer. Those studies are definitive.
Q: 47 yo female had first mammo 7 years ago at age 40. Was told during first mammogram that I would need to stay in the office to have ultrasound. Had ultrasound and was advised I had calcification on chest wall. Had to return in 6 months for follow up mammogram, no changes. What is calcification and what causes it? Do I need to worry about any complications from the calcification in the future?
Dr. Severt: Calcification is a sign of your body “cleaning something up.” It is kind of what it sounds like. When hard water is on the counter and dries, it leaves a white residue, a salt. When things in the body are “drying up,” they can leave behind a calcium deposit. Chest wall calcification is typically found after an injury, or can be due to problems in the skin. It does not increase the risk of breast cancer or any other cancer. We look for calcifications in the breast as a sign of early cancer, or ductal carcinoma in situ (DCIS). The reason we look closely at all calcifications on mammography is because some specific kinds of calcification are signs of an early breast cancer. We get magnification views to get a good look at these things so we can tell what might be the cause.

Photo: Rhoda Baer
Q: I’m 50 years old and had a mammogram earlier this month. It was extremely painful and I bruised. Why does it hurt so much!? It made me not want to have another one in a year!

Leah Hahn
Leah Hahn: Although it can sometimes be uncomfortable, compression to the breast is necessary to spread the breast tissues apart, reduce the amount of radiation, and to decrease blurring from motion. We do achieve better images with breast compression.
The pressure from compression isn’t harmful, but you may find it uncomfortable or even a little painful. It is possible to have some bruising after a mammogram. A mammogram should not hurt so much that it deters future tests. If you have too much discomfort, tell the technologist. Many sensitive technologists are willing to take their time to reduce pain.
Dr. Severt: Ouch. On behalf of all mammographers, I apologize. Some women have sensitive breasts. However, bruising is not a sign of sensitivity, it is a sign of damaged blood vessels. If this was a one-time occurrence, if you’re not bleeding or bruising from activities like brushing your teeth, then it was probably a zealous technologist applying a little too much force on the compression paddle. If you are bruising and bleeding easily, see your doctor. You may need other tests.
Q: How do techniques and frequencies change for patients with BRCA-1 gene, including both men and women?
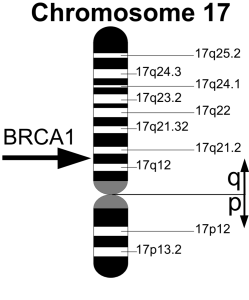 Dr. Severt: Frequency for mammography is the same, once per year. Consider interleaving MRI at yearly intervals so that you are getting one of these tests every six months.
Dr. Severt: Frequency for mammography is the same, once per year. Consider interleaving MRI at yearly intervals so that you are getting one of these tests every six months.
Q: When is MRI instead of mammography appropriate?
Dr. Severt: We use MRI as an adjunct to screening mammography when your lifetime risk of developing breast cancer is over 20%. People with genetic predisposition to breast cancer fall into this group. We also use breast MRI prior to surgery for breast cancer in order to better plan that surgery and avoid missing unexpected lesions, especially lesions in the other breast.
Q: My mammogram in August was “Computer-Aided Detection and breast tomosynthesis.” How does this compare to 3D? Insurance fully covered it. Mother at 70 and sister at 58 both had breast cancer, so I have had annual mammogram for more than 20 years.
Dr. Severt: Computer aided detection – CAD – is also called a computerized second look system. We almost all use that to help read mammograms. Tomosynthesis is 3D – those terms are synonymous. Tomosynthesis is the generic medical name for the technology, 3D is the term used more in advertising. Thank you for getting your mammogram!
Q: Based on your comments regarding the low radiation of a mammogram, would it be reasonable to have one done every six months rather than annually, if I wanted to?
Dr. Severt: There is no recommended schedule for getting mammograms every 6 months. Part of reading mammograms is looking for changes. These are slow changes, and getting a study every 6 months could actually make it more difficult to interpret your mammogram! Strange but true.
Q: What can you tell us about men and breast cancer?
Dr. Severt: Men have ducts under the nipple and they can get breast cancer. The lifetime risk for a man to develop breast cancer is about 1 in 1000. In women it is 1 in 9. It’s uncommon, but it can happen. Check out the American Cancer Society for more info about men and breast cancer.
Q: What causes a very slow discharge, that shows up on the bra, throughout the day? I had a breast exam . . mammo will be on Wednesday.
Dr. Severt: Lots of things. If the discharge is bloody, could be blood by products, usually black, or is clear, we worry about it. If it is green, yellow, milky or probably milky, we do not worry about it as being caused by something in the breast. Breasts discharge can be caused by nipple stimulation, certain medications and even brain tumors (although brain tumor is one of the least likely causes).
Q: What’s with the dense breast disclaimer my friends and I have received lately? We aren’t being referred anything exact as a next step.
Dr. Severt: In 2011, Minnesota adopted a state law requiring accredited mammography sites to include in the letter a statement about breast density when a patient’s mammogram is judged to be one of the top two levels of density. There are 4 levels in total. Anyway, the legislature gave us the exact words that we must include and did not allow for any extemporaneous creative writing to be added. You get what your lawmaker said we have to say. Your next step is to continue annual mammography, seek a site with 3D mammography, which is better for dense breasts. Some sites add whole breast ultrasound, which also sees through the dense tissue better.
Q: What are dense breasts and what is the best imaging for them?
Dr. Severt: Breasts are made up of fatty tissue and everything else. The everything else is ducts, acini where the milk is produced, ligaments and connective tissue. In general, fatty tissue passes x-ray better than everything else. It looks black or dark on mammogram. Everything else looks light gray and white. Breast cancer is usually white or close to white. It is much easier to spot in the middle of a fatty breast. I addressed imaging in the last answer, but it is 3D mammography plus or minus whole breast ultrasound. If you are at a greater than 20% lifetime risk of developing breast cancer, think about adding breast MRI.
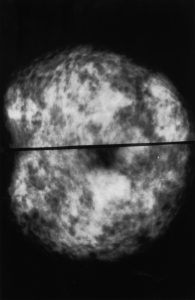
Normal mammogram – dense breasts
From National Cancer Institute
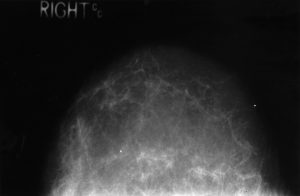
Normal mammogram –
fatty breast
From National Cancer Institute
From Dr. Hilden: To compare dense breasts with fatty breasts, look at these two mammograms in the above pictures – both read as normal. Now if you know that cancer usually appears white, which mammogram do you think it more likely than a cancer could hide in? The dense ones. All the disclaimers and discussion about dense breasts is due to this possibility.
I hope you’ve learned something from this discussion about mammograms. I want to thank Leah Hahn and Dr. Tony Severt for lending us their expertise!

Tony Severt, MD & Leah Hahn
Full service radiology!
One more thing . . . breast care at HCMC is about to go from outstanding to simply awesome. Coming on March 26, 2018 as part of Hennepin’s new Clinic and Specialty Center, the Wanzcek Family Breast Care Center will be open for business. State-of-the-art breast imaging in a convenient and patient-focused new center. More info available at the Clinic and Specialty Center page.
Subscribe by e-mail for notifications from this blog (no spam, I promise) and follow me on Twitter @DrDavidHilden
-David

